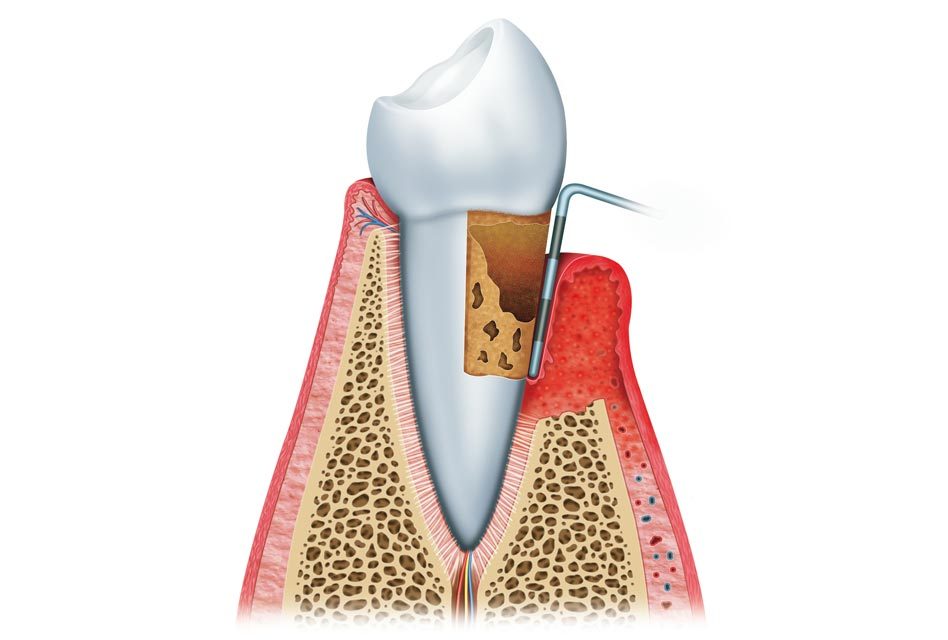
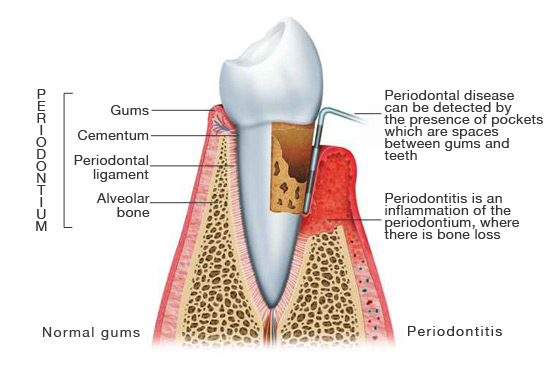
Periodontitis is an inflammatory disease that affects the periodontium, which is the group of all the tissues that surround and support teeth. Among these tissues, the periodontium is made of the alveolar bone, the gums, the periodontal ligament and the cementum.
Periodontitis is therefore a progressive loss of alveolar bone around teeth. If periodontitis is not treated, teeth begin to move and eventually fall out.
This disease is mainly caused by microorganisms (harmful bacteria and protozoa), and an aggressive response of the immune system against these microorganisms. The dentist makes the diagnosis by detecting the presence of periodontal pockets (spaces created between the gums and the teeth) and the analysis of X-rays to evaluate bone loss.
Classification
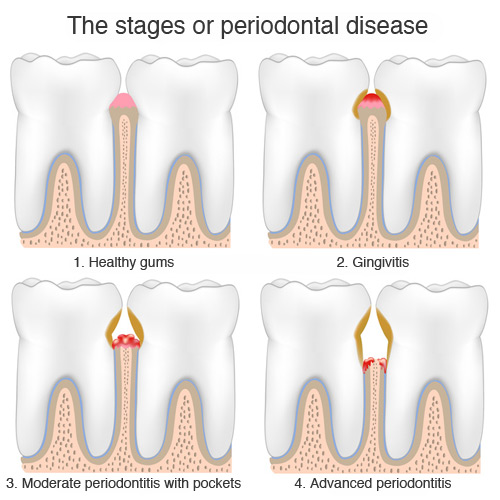
Periodontitis is part of a group of gum diseases that affect the periodontium at different levels. Gingivitis is the first stage, and it’s expressed by inflammation of the gums on the surface only without touching the alveolar bone. Gingivitis can be cured by proper methods of oral hygiene.
When inflammation and infection reach the periodontium in a deeper manner, the disease is called periodontitis. There are several stages of periodontitis, which depend on how much tissue, and alveolar bone was destroyed. A periodontal pocket is a space between a tooth and the gum around it. By measuring pockets at six sites around each tooth, the dentist can get an idea of the destruction of bone and the severity of periodontitis:
- a pocket of 1-2 mm is considered normal;
- a pocket of 3 to 4 mm means beginning periodontitis;
- a pocket of 5 to 6 mm means moderate periodontitis;
- a pocket of 7 mm and more means severe periodontitis.
A pocket can be misinterpreted if there is gum recession. When there is recession, the gum has receded and teeth look longer. In these cases periodontal pockets may be less deep although there is significant destruction of alveolar bone.
Another case where a pocket might be misinterpreted is when there is gingival hyperplasia. This rare condition is defined by gum swelling that grows over a tooth making it look shorter. Hyperplasia might therefore create a gingival pocket without there being loss of alveolar none.
Another way of classifying periodontitis is to designate it as being localised periodontitis if only a few teeth are affected (<30%), and generalized periodontitis if multiple teeth are affected (> 30%).
Signs and symptoms
 Unless there is pain and bleeding, the early stages of periodontitis show few symptoms. The disease has generally progressed when a person consults a dentist.
Unless there is pain and bleeding, the early stages of periodontitis show few symptoms. The disease has generally progressed when a person consults a dentist.
Here are the main symptoms of periodontitis, which are mostly painless, even though the disease is progressing:
- bleeding gums while brushing, flossing, or eating hard foods like apples; this can also happen when a person is suffering from gingivitis without having reached the stage of periodontitis;
- swollen gums;
- halitosis (bad breath) or a metallic taste in the mouth;
- gum recession can be observed by having longer teeth; gum recession can also happen when someone uses a toothbrush too vigorously;
- loose teeth.
Effects of periodontitis that can occur elsewhere than in the mouth
 Periodontitis is a chronic infection, which weakens the human body because a person is constantly trying to fight the inflammation. Moreover, harmful microorganisms that attack the gums can also reach other organs in the body.
Periodontitis is a chronic infection, which weakens the human body because a person is constantly trying to fight the inflammation. Moreover, harmful microorganisms that attack the gums can also reach other organs in the body.
More and more scientific studies prove that chronic periodontitis has the following effects:
- aggravate cardiovascular disease;
- make diabetes worse, because systemic inflammation caused by periodontitis decreases the ability of balancing glucose in the blood;
- reversibly, people with diabetes are more susceptible to periodontal disease because diabetes reduces resistance to infection;
- deteriorate memory and mathematical mental abilities for people of age 60 and over.
Causes
In most cases periodontitis begins with gingivitis, which is an infection and inflammation of the superficial part of the gum. If gingivitis is left untreated, the infection can eventually reach and destroy the alveolar bone and create pockets.
The main causes of periodontitis:
- poor oral hygiene;
- deficient nutrition;
- systemic diseases such as diabetes;
- smoking;
- tartar around teeth that is not regularly cleaned professionally by a dentist or hygienist.
Prevention
 Prevention is the best way to avoid periodontal disease because it’s a disease that is very difficult to control. Here are ways to prevent (not cure) periodontitis:
Prevention is the best way to avoid periodontal disease because it’s a disease that is very difficult to control. Here are ways to prevent (not cure) periodontitis:
- good oral hygiene which includes brushing and flossing on a daily basis;
- using mouthwash in combination with brushing and flossing by rinsing with either salted water or a solution of chlorhexidine; mouthwash can cure gingivitis but cannot cure periodontitis;
- regular professional cleanings by a dentist or hygienist to remove tartar; regular check-ups to examine if there is alveolar bone loss or periodontal pockets.
Treatments
Note that for successful treatment it is essential to establish excellent hygiene. It is important to understand that after any treatment, a person with chronic periodontitis must follow these hygiene measures for the rest of his or her life. Periodontal treatment in combination with appropriate hygiene measures, only stabilise periodontitis, they do not heal it completely. But it’s important to remember that all this effort is valid in order to keep your teeth.
Here’s a summary of the stages of periodontitis treatments:
- Curettage – Also known as root planning or deep cleaning, this procedure cleans the tartar, plaque and any residual finding themselves under the gum. Although this is not surgery, it is best to use local anaesthesia to make it comfortable. Most research has concluded that this procedure successfully treats periodontal pockets of less than 5 mm.
- Revaluation – About three months after treatment, we must reassess the methods of hygiene and the condition of the gums. The bags are re-measured and compared with the initial steps. With deep pockets still bleeding on probing indicates that periodontitis is always present in an active and that the bone will continue to destroy time.
- Surgery – If after the reassessment there were still teeth that have active signs of the disease, surgical treatment would be indicated. There are several surgical approaches exist, ranging from open curettage of bone regeneration with a matrix. The purpose of all these approaches and to correct irregularities of the alveolar bone and reduce the depth of periodontal pockets. Treatment with surgery, together with good hygiene, has a good success rate, can prevent tooth loss up to 85%.
- Maintenance – To keep the successful long-term treatment of the gums, maintains continuous therapy should be respected. This includes professional cleaning of his teeth every three months to remove any tartar that may develop. The oral hygiene at home is as important including brushing and flossing daily. If these measures are not met, there may be accumulation of tartar and plaque, and periodontitis can return actively.
References
- Wikipedia, the free encyclopedia (www.wikipedia.org).
- Mayo Clinic, medical information and tools for better living (www.mayoclinic.com).
The information above should be used as a reference only. Any medical decision should not be taken before consulting a health care professional.
The masculine gender may have been more used in the article, but without prejudice, to make reading easier.
Category dental problems
- Abfraction
- Abrasion
- Ankylosis
- Anodontia
- Attrition
- Broken fillings
- Bruxism (Teeth Grinding)
- Cavity (tooth decay)
- Cold sore (herpes labialis)
- Dental abscess
- Dental plaque
- Denture Irritations and Infections
- Denture stomatitis (prosthetic stomatitis)
- Dry socket
- Erosion
- Fluorosis (dental)
- Gingival hyperplasia
- Gingival pocket
- Gingivitis
- Gum Disease (Periodontal Disease)
- Gum recession
- Halitosis (Bad Breath)
- Hyperdontia (supernumerary teeth)
- Hypocalcification
- Hypodontia
- Impacted tooth (tooth impaction)
- Leukoplakia
- Lichen planus
- Malocclusion (Misaligned Teeth)
- Microdontia
- Micrognathia (micrognathism)
- Mucocele
- Oligodontia
- Oral cancers
- Oral candidiasis
- Overbite
- Overjet
- Pericoronitis
- Periodontal pocket
- Periodontitis
- Prognathia (prognatism)
- Resorption
- Retrognathia (retrognatism)
- Sleep apnea
- Tartar (Calculus)
- TMD (Pain and Cracking of the Jaw)
- Tooth Discolouration
- Tooth sensitivity (sensitive teeth)
- Torus
- Trismus
- Ulcers and canker sores
- Xerostomia (Dry Mouth)